Originally published in 2019, and updated in 2023 (see end of post for update)
I am a birth educator. I also have a PhD in physiology of reproduction, and 20 years of research experience and I have a confession to make: I get REALLY irate when women get given poor quality evidence (or no evidence at all) in support of a recommendation for inducing labour.
Whether I’m wearing my doula hat, or my scientist hat, I have to admit to getting really fed up with the growing epidemic of induction of labour for dubious reasons. This article is going to explore one of the most common stated reasons for induction of labour at term : The idea that labour should be induced before a certain point in pregnancy is reached because the ‘older’ placenta is not as efficient.
I want to clarify one thing before we start: I am NOT anti induction, when it is justified by solid medical evidence and when a woman weighs up the evidence and decides that the risk of continuing the pregnancy is higher than the risk of inducing labour (like for example pre-eclampsia or reduced fetal movements, or when there are psychological reasons for the woman to choose to be induced).

Over the last 15 years, between teaching antenatal classes and supporting women a a doula, I have heard and witnessed hundreds of stories of induction, the majority of which ended up being traumatic for the mother.
In my area of work we often refer to this as the “car crash”, which goes something like this: 3 days of prostaglandin induction (often made more stressful because the woman cannot be with her family for much of the time), followed by 24 hours of syntocinon and a caesarean at the end for either fetal distress or “failure to progress” (if only women were told : We’re really sorry, we didn’t manage to get you into labour with our drugs, so now the only option is a cesarean, maybe women wouldn’t feel as traumatised as when they are labelled a failure. Language matters).
I have listened and held women (and their partners) as they told me of their upset, their grief, their disbelief, lack of preparation and their feelings of failure.
One of the top quoted reasons for inducing women when pregnancy goes beyond 41 weeks is the idea that the placenta somehow stops working after pregnancy reaches a certain number of weeks.

The implication is that the placenta has a sell by date, like a piece of meat in the supermarket.
Recently yet more papers have been published claiming as a fact that placentas “age”, “degrade” and “fail” in older mothers and after a certain number of weeks of pregnancy.
I don’t normally like to write solely about science stuff these days. I like to write about how I feel about issues, and stick a few references in for people who want to read them. I spent 20 years doing scientific research in the academic and industry setting. I’ve moved on from this, I find most of the scientific world too dry and frankly, too blinkered.
But I’m losing patience with this so-called science causing so much damage to women.
I was very concerned a few weeks ago to watch a heated debate on social media about this topic; seeing many of my colleagues being gaslighted into believing the so-called science by people who claim to have all the answers, using jargon that they do not understand.
I believe that my scientific background combined with my experience as antenatal educator and doula gives me a unique, broad perspective on this topic.
So it’s time to put my scientific hat back on, analyse the papers in question, and offer my rather alternative interpretation of the current evidence, so that women and birth workers can make truly informed decisions, not one-sided ones based on the opinions of a few so-called experts whose views are based on their existing belief and opinion rather than a considered weighing-up of the evidence in this area.
I suggest you grab yourself a cup of tea, because this is going to be a long one!

Before I start I want to make an important point: even experts in a field often disagree with one another.
When I was working in the academic field during my PhD and 2 postdocs, working in a small niche area of biology research (clock genes, the genes which control rhythms, such as waking and sleeping), I published in fairly high ranking scientific papers, and became quickly perceived as an expert in my field. This led me to be invited as a guest speaker at conferences. I remember arguing until I was blue in the face about the interpretation of certain data with other experts in the field. It was done passionately, but it was entertaining, good humoured and fun. It happened because, as I will explain below, good scientists understand that science isn’t black and white.
The conversations I see on social media about this research aren’t like this. I see experts pretending to have all the answers, presenting themselves as the only ones who have all the knowledge, and frankly bamboozling and bullying non scientists with jargon.
In this particular case, they take the moral high ground, presenting themselves as saviours, as if stillbirths could be guaranteed to be prevented if only we induced all women at a certain number of weeks of pregnancy. They attack other people whose views are different, even when these people are equally or more qualified and hold PhDs in relevant fields.
This isn’t right. This harms women, and this harms the people who are supporting them too.
Even in science, things are never black and white. Nothing is guaranteed. There are many shades of grey. And pretending that things are this way isn’t science, it is delusion, and it is treating science as a dogma. If you want to find out more about this way of thinking, watch Cambridge scientist Dr Rupert Sheldrake’s banned TED talk on the topic.
Now that’s out of the way, back to the subject at hand: do placentas really age? Do they stop functioning correctly towards the end of pregnancy? And most importantly, are they solely responsible for the (let’s remember, tiny) rise in stillbirth towards the end of pregnancy? These are the assumptions that currently underpin our induction policies.
I feel I need to explain first that the risk of increased stillbirth at term, which is the main reason behind induction policy, is actually very small, rising from about 0.1% (1 in a 1000) at 40-41 weeks, to about 0.3% (3 in a 1000) at 42 weeks and about 0.5% (5 in a 1000) at 43 weeks (from this paper). The Cochrane review on induction beyond term , found that induction before 42 weeks reduced the risk of perinatal death from 0.3% to 0.03%, and that the authors of the review concluded that:

” A policy of labour induction compared with expectant management is associated with fewer perinatal deaths and fewer caesarean sections. Some infant morbidities such as meconium aspiration syndrome were also reduced with a policy of post-term labour induction although no significant differences in the rate of NICU admission were seen. However, the absolute risk of perinatal death is small. Women should be appropriately counselled in order to make an informed choice between scheduled induction for a post-term pregnancy or monitoring without induction (or delayed induction).”
In practice I almost never see the part highlighted in bold being presented as an option to women (read my previous blog about it here)
I would like to quote the seminal paper by the late Dr Fox “Aging of the placenta“
” A review of the available evidence indicates that the placenta does not undergo a true aging change during pregnancy. There is, in fact, no logical reason for believing that the placenta, which is a fetal organ, should age while the other fetal organs do not: the situation in which an individual organ ages within an organism that is not aged is one which does not occur in any biological system. The persisting belief in placental aging has been based on a confusion between morphological maturation and differentiation and aging, a failure to appreciate the functional resources of the organ, and an uncritical acceptance of the overly facile concept of “placental insufficiency” as a cause of increased perinatal mortality.”
Whilst I am fully aware that this paper is dated, having being published in 1997, and that much more research has been carried out since, I still believe his conclusion stands, the last sentence in particular.
I’ve heard many maternity care providers coerce expectant mothers to accept induction (remember, if you feel coerced, this isn’t consent) to the cries of “your placenta is failing right now”. Yet, even today, we do not know what accounts for the tiny rise in neonatal mortality after 40 weeks.
There seems to be a strong desire to prove the causality between placental aging and the increase in stillbirth and this desire is guided by a positive drive, which is to reduce stillbirth.
I empathise with this drive better than you know, because my younger brother was stillborn so I fully understand the devastating effects the death of a new baby has on a family.
But for the moment it’s just this: a theory.
And anyone can invent a theory about anything, but that doesn’t make it true.
We need to find a balance between the real statistics and women’s wishes for a positive birth experience. Because there is no doubt from the evidence in this area that, as long as mother and baby are well, it is better for all involved for labour to start on its own.
Because we mustn’t forget that inductions can be very traumatic for women and they can cause fetal distress in babies.
It’s quite simple, really: let the mothers decide what they want. And for this, they need real facts and numbers, not emotive coercion.
First, a bit of history
How did the whole concept of placental failure ever come about?
In her book “Inducing labour, making informed decisions” , Dr Sara Wickham explains that this theory came about first via the work of Ballantyne who described a wasting condition of the newborn in 1902, followed by Runge in 1958 who coined the term placental insufficiency. This became known as the Ballantyne-Runge syndrome, and led to the assumption of a relationship between the length of pregnancy and placental failure.
Dr Wickham goes on to explain that this theory has never been proven and that there is no evidence behind it. She explains that, while we know that some women’s placentas do sometimes fail to provide sufficient nutrients for their baby, this doesn’t mean that all women’s placentas routinely fail at a certain point in time. Further evidence of how much those who are challenging this theory really do care about the wellbeing of babies can be seen where Dr Wickham notes in her talks that the concern is not just about preventing unnecessary inductions for women who do not need them. By trying to make standardised, population-level recommendations (or a ‘one size fits all’ approach), we not only lead many women to have inductions that they do not need, but we may also fail to identify and help the small number of babies who truly do need help but at a point earlier than the current population-level cut-off point for induction.
Even in the papers claiming that there is a relationship between the length of pregnancy and the state of the placenta, when you dig into them, the conclusion reached is always that there is a “possible link” rather than a proven one.
And as I explained before, experts in the field do not agree with one another. In her book “Why induction matters“, Dr Rachel Reed quotes a couple of prominent papers, in particular a paper by Maiti et al which claims a direct link between placental aging and stillbirth, and a paper by Mazzurato et al ” Guidelines for the management of postterm pregnancy” which states that:
” Although the fetal, maternal and neonatal risks increase beyond 41 weeks, there is no conclusive evidence that prolongation of pregnancy, per se, is the major risk factor. Other specific risk factors for adverse outcomes have been identified, the most important of which are restricted fetal growth and fetal malformations. In order to prevent PT (Post term) and associated complications routine induction before 42 weeks has been proposed. There is no conclusive evidence that this policy improves fetal, maternal and neonatal outcomes as compared to expectant management.”
The nitty gritty of the arguments behind the aging placenta theory
Some of the technical terms I see bandied around a lot, and which bamboozle many of my colleagues because they do not understand their meaning, are morphological changes in the placenta such as apoptosis, autophagy, syncytial knots, reduction in telomere length and so on. In many papers, the authors claim that these are key features of aging, and observed in post-term placentas.

Yet there is more than one interpretation of these morphological changes so often lauded as proof of a placental ‘sell-by date’. They do not automatically mean that there is a problem. In many ways, our understanding of this area is in its infancy, and we would do better to take a position of scientific humility while we try to determine the meaning of these findings.
One of the most striking examples of a study which makes suggestions that aging of the placenta at term is a fait accompli is this study, with its sensational title: “Evidence that fetal death is associated with placental aging” by Maiti et al.
I find one of the statements in this paper extremely concerning:
” The known exponential increase in unexplained intrauterine death that occurs >38 weeks of gestation may therefore be a consequence of aging of the placenta and decreasing ability to adequately supply the increasing needs of the growing fetus. This knowledge may impact on obstetric practice to ensure infants are born before the placenta ages to the point of critical failure“
I fear such a statement will be used to pressure yet more women into being induced earlier, without any concerns for their personal decision or well being. And yet, as I will keep saying, this is still an unproven theory and different experts have different opinions about whether it is true or not. The medical profession is based on the tenet of ‘first do no harm’ and my understanding is that this means that we should not intervene unless we have good evidence to support doing so.
I will go through clarifying the differential interpretation of some of the changes observed in the placenta.
One of the changes they observe in this paper is decreased autophagy. Autophagy is a kind of cellular recycling system. The authors infer that these changes are a proof of aging. Yes, autophagy decrease has been associated with aging in some studies. Some other authors, however, are suggesting that the reduction in autophagy in the placenta may be part of the process that actually starts labour and so it may be a normal and important part of a physiological process rather than a sign that something is ‘wrong’.
Another placental change, quoted in the paper by Maiti cited above, is apoptosis (also known as programmed cell death). Apoptosis isn’t just a proof of senescence (aging). Apoptosis also happens during fetal development and during adolescence. It is as much as sign of change as it is a sign of ageing, and of course change and growth are very important at this time; the whole point of pregnancy is that the baby grows and changes
“The role of apoptosis in normal physiology is as significant as that of its counterpart, mitosis. It demonstrates a complementary but opposite role to mitosis and cell proliferation in the regulation of various cell populations. It is estimated that to maintain homeostasis in the adult human body, around 10 billion cells are made each day just to balance those dying by apoptosis (Renehan et al., 2001). And that number can increase significantly when there is increased apoptosis during normal development and aging or during disease.”
And during pregnancy
“Trophoblast apoptosis is a physiologic event in normal pregnancy, increases with advancing gestational age and is higher in post- term pregnancies and therefore is considered as a normal process in the development and ageing of the placenta.”
Again and again we see that the processes which are claimed by some to be evidence of aging could also be interpreted to be signs of the normal growth and change which are the very function of pregnancy.
Syncytial knots (SNAs, an accumulation of cell nuclei (the centre of cells) inside placenta cells) are another change quoted as a proof of ageing:
” SNAs may form to structurally reinforce the placenta and minimise damage from shear stresses or other mechanical sources, reduce the proportion of nuclei in highly active vasculo-syncytial membranes or result from cell turnover in the placenta without an apoptotic trigger or shedding process. Ultimately, a better understanding of the processes leading to SNA formation will give insight into their significance in pregnancy complications.”
So again, what we are seeing could just as well be an adaptation rather than a sign of ageing.
“Telomeres, the DNA–protein structures located at the ends of chromosomes, have been proposed to act as a biomarker of aging. In this review, the human evidence that telomere length is a biomarker of aging is evaluated. Although telomere length is implicated in cellular aging, the evidence suggesting telomere length is a biomarker of aging in humans is equivocal. More studies examining the relationships between telomere length and mortality and with measures that decline with “normal” aging in community samples are required. These studies would benefit from longitudinal measures of both telomere length and aging-related parameters.”
In this paper called “Questioning causal involvement of telomeres in aging” the authors state:
“Multiple studies have demonstrated that telomere length predicts mortality and that telomeres shorten with age. Although rarely acknowledged these associations do not dictate causality. In addition, the causality hypothesis assumes that there is a critical telomere length at which senescence is induced. This generates the prediction that variance in telomere length decreases with age. In contrast, using meta-analysis of human data, I find no such decline. Inferring the causal involvement of telomeres in aging from current knowledge is therefore speculative and could hinder scientific progress.”
What I find of particular interest, is that the authors of this paper also speculate that these cellular changes may form part of what starts labour:
” Placental senescence raises several important questions that need to be addressed experimentally. While fusion-induced senescence appears to be required for syncytiotrophoblast formation, it is likely that senescence of both fetal tissues and the maternal decidua play at least a part in determining timing of labour onset”
So what if what is seen in the placenta and interpreted as a sign of aging, are in fact normal, healthy changes, which are a sign of healthy growth and development and which may also play a role in the start of labour?

Another “older” sign of placental aging is calcifications. I’ve been guilty myself of believing people who told me it was a sign of ageing and it was good that the baby had been born because the placenta was “old”. I recently came across this blog (which has published references to back up all its claims):
“So while calcification of a placenta at term – around 39-42 weeks is part of the normal appearance of a full-term placenta and has no clinical significance in a healthy pregnancy, the appearance of significant calcification earlier in pregnancy is associated with risks to both the mother and baby. Just like we would be concerned about a very young person with wrinkles – it could be a sign of something significant happening (…) So, in essence, when a mother is healthy and full term, calcification and infarcts are normal features of a healthy placenta – just like your healthy mother has some wrinkles and a few grey hairs.
Yet another myth blown out of the water.
In conclusion, whilst there is evidence of cellular changes in the placenta throughout the course of pregnancy, there still isn’t any solid evidence to prove that it is indeed aging rather than an adaptation, or that these changes are truly accountable for the tiny rise in stillbirth when pregnancies continue beyond 42 weeks.
The concept of the aging placenta is still just that, a theory. Unfortunately the majority of the publications cited in this post fail to acknowledge this, and take this theory as proven.
What worries me even more, is that no consultation of women’s view on the induction process usually takes place, and these publications will form the basis of the new NICE guidelines, then the local hospital guidelines, and therefore more and more women will be induced needlessly, and have negative or traumatising experiences.
This is underpinning a current trend towards inducing women even earlier, at 39 weeks instead of the current 41 to 42 weeks.
Evidence based birth has produced an excellent review of the literature on this topic.
I hope that reading this blog will help families and their supporters make informed decisions.
I also would like to encourage scientists and policy makers to stay curious about the wider picture and to engage more with pregnant women and their views on the induction process.
Update August 2023
Having reviewed more recent evidence since I published the blog in 2019, I still stand by what I wrote above. I cannot see anything in the more recent literature that has changed. What strikes is that all the research is looking at proving that placentas age, but no one is looking at it from another angle: the fact that it made simply be changes, a process of maturation, necessary as part of the birth process. This is a case of culture leading science. As Dr Sara Wickham says :
“our modern culture is not very tolerant of the concept of aging generally, especially in women, so it is not that surprising that we so easily accept the idea that the aging placenta is unwanted and problematic.”
A review paper in 2020 called “A review of the Evidence for Placental Ageing in Prolonged Pregnancy“, whilst it makes a case for the so-called aging, also states this in the discussion:
“Given the close relationship between placental structure, cell processes and placental function these changes would be expected to lead to a reduction in placenta function. However, we have not been able to identify any studies which have examined this link.”
My review of the latest evidence led me to find a paper called Aging of the Placenta, published in the journal Aging in 2022. The paper contained the following paragraph :
“As gestation progresses, the placenta undergoes senescence. Generally, this process is necessary to detach the placenta from the uterine wall following parturition, eventually allowing blood vessels to close (to prevent haemorrhage) and the uterus to regain pre-pregnancy size and shape”
I researched this and found publications that show that the very processes that the publications that talk about aging describe: inflammation, apoptosis, may actually be part of the normal process the placentas need to do to detach.
Therefore my suggestion that what is interpreted as aging may be a normal physiological and maturation process now has some evidence behind it.
This also made me wonder: If we induce labour, may we be interfering with this maturation process, and would induction results in more difficulties birthing the placenta? Reading around this subject shows that induction of labour is a known risk factor for retained placenta.
Feel free to signup to receive my newsletters by using the signup form at the bottom of this page
A Note to Readers
Thank you for reading my article on The Myth of the Aging Placenta. While I’m passionate about sharing evidence-based information on this topic, please note that I cannot provide personalised support or respond to individual questions in the comments section.
For those seeking individualised guidance related to pregnancy and birth, whether you are pregnant or a birth professional, I offer individual mentoring sessions, as well as mentoring packages. During these sessions, I can offer more tailored information based on your specific situation.



 I tell you what, since you’re both still kind of low risk, as long as you’re still under 25 by the time you have sex, we could let you go to our Natural Climax Centre, instead of the Intimacy Unit. It’s a home from home centre, with large rooms, double beds and mood lighting, and even one hot tub per room so you can get in the mood and relax. It looks more like a fancy B&B than a hospital! It’s staffed by experienced intimacy midwives, who are skilled in supporting physiological sex. So it will be just yourselves, a midwife, and a couple of reproductive students. They only use intermittent monitoring every 5 min during the established arousal phase. Of course if anything goes outside of the guidelines, we would suggest you transfer to the Intimacy Unit where we can monitor your heart rate continuously, as well as intervene with a penis substitute if you cannot finish by yourself. As I said before, as you have an untried penis, we don’t know which way it will go.
I tell you what, since you’re both still kind of low risk, as long as you’re still under 25 by the time you have sex, we could let you go to our Natural Climax Centre, instead of the Intimacy Unit. It’s a home from home centre, with large rooms, double beds and mood lighting, and even one hot tub per room so you can get in the mood and relax. It looks more like a fancy B&B than a hospital! It’s staffed by experienced intimacy midwives, who are skilled in supporting physiological sex. So it will be just yourselves, a midwife, and a couple of reproductive students. They only use intermittent monitoring every 5 min during the established arousal phase. Of course if anything goes outside of the guidelines, we would suggest you transfer to the Intimacy Unit where we can monitor your heart rate continuously, as well as intervene with a penis substitute if you cannot finish by yourself. As I said before, as you have an untried penis, we don’t know which way it will go.
 When I worked as a doula, I used to gift a rebozo to my clients as part of my doula package, this way I knew they were more likely to become familiar with it and use it, plus it would make a lovely thing to keep afterwards. I would teach the partner a bunch of support and relaxation techniques, as well as show the mother how to wrap her belly and hips. A standard length (2m) works well for most people. I once supported a petite pregnant woman to wrap her hips, and I brought an long 2.5m instead of a 2 m one by mistake, and there was so much fabric around her hips when we practiced wrapping, making it feel cumbersome, so I brought her a shorter one at the next visit. However if the woman or her partner is tall then a longer rebozo might be more comfortable to use.
When I worked as a doula, I used to gift a rebozo to my clients as part of my doula package, this way I knew they were more likely to become familiar with it and use it, plus it would make a lovely thing to keep afterwards. I would teach the partner a bunch of support and relaxation techniques, as well as show the mother how to wrap her belly and hips. A standard length (2m) works well for most people. I once supported a petite pregnant woman to wrap her hips, and I brought an long 2.5m instead of a 2 m one by mistake, and there was so much fabric around her hips when we practiced wrapping, making it feel cumbersome, so I brought her a shorter one at the next visit. However if the woman or her partner is tall then a longer rebozo might be more comfortable to use. If you are tall (over 5ft6, 1.67m) and you want to use your rebozo to do floor techniques (for example, to rock someone’s hips whilst they lie on the floor), then with a 2 m length you will need to bend forward as you work, which can be uncomfortable. A longer length (2.5m) might work better for you. Similarly, if the person you are supporting is very curvy, a short rebozo might not be long enough to cup the hips comfortably. Much of this is also down to personal preference and experience.
If you are tall (over 5ft6, 1.67m) and you want to use your rebozo to do floor techniques (for example, to rock someone’s hips whilst they lie on the floor), then with a 2 m length you will need to bend forward as you work, which can be uncomfortable. A longer length (2.5m) might work better for you. Similarly, if the person you are supporting is very curvy, a short rebozo might not be long enough to cup the hips comfortably. Much of this is also down to personal preference and experience. Open weave rebozos lend themselves very well to wrapping. The open weave means that they cup the body really closely, which is great for rocking and massage. When I trained with Mexican midwife Naoli Vinaver, she favoured these as well. They are also very grippy which means they stay tucked when wrapped around the body. They are my favourite rebozo for closing the bones. They are also thinner and pack smaller. The open weave can make them prone to pulls, so they are more fragile than closed weave rebozos, but thread pulls are easily pulled back into the weave by tugging on the fabric. For closing the bones I use 2m ones for the head, ribs, legs and feet, and 2.5 m ones for the shoulders and hips as they are the widest part of the body.
Open weave rebozos lend themselves very well to wrapping. The open weave means that they cup the body really closely, which is great for rocking and massage. When I trained with Mexican midwife Naoli Vinaver, she favoured these as well. They are also very grippy which means they stay tucked when wrapped around the body. They are my favourite rebozo for closing the bones. They are also thinner and pack smaller. The open weave can make them prone to pulls, so they are more fragile than closed weave rebozos, but thread pulls are easily pulled back into the weave by tugging on the fabric. For closing the bones I use 2m ones for the head, ribs, legs and feet, and 2.5 m ones for the shoulders and hips as they are the widest part of the body. Closed weave rebozos are both beautiful, grippy and sturdy. Most of them are soft straight away (though depending on the weaver some may need more than a wash and some use to soften the fabric, a bit like with a brand new babywearing woven wrap), and the closed weave makes them less prone to pulls and broken threads. They are slightly thicker than open weave rebozos. They are an all round versatile sturdy rebozo, and they make a good baby carrier too (here is a bunch of
Closed weave rebozos are both beautiful, grippy and sturdy. Most of them are soft straight away (though depending on the weaver some may need more than a wash and some use to soften the fabric, a bit like with a brand new babywearing woven wrap), and the closed weave makes them less prone to pulls and broken threads. They are slightly thicker than open weave rebozos. They are an all round versatile sturdy rebozo, and they make a good baby carrier too (here is a bunch of 
 Why does wrapping helps?
Why does wrapping helps? I had ever heard of rebozo or using the shawls to wrap your hips and thought that anything was worth a try as I am in such horrendous pain. Since using the wrap I have been able to do shopping and walk around without crying in pain, it makes a huge difference, so easy to use, looks pretty and I love that I can use it during labour and after as a sling! Hannah
I had ever heard of rebozo or using the shawls to wrap your hips and thought that anything was worth a try as I am in such horrendous pain. Since using the wrap I have been able to do shopping and walk around without crying in pain, it makes a huge difference, so easy to use, looks pretty and I love that I can use it during labour and after as a sling! Hannah My
My  What can you use to wrap your hips and belly?
What can you use to wrap your hips and belly?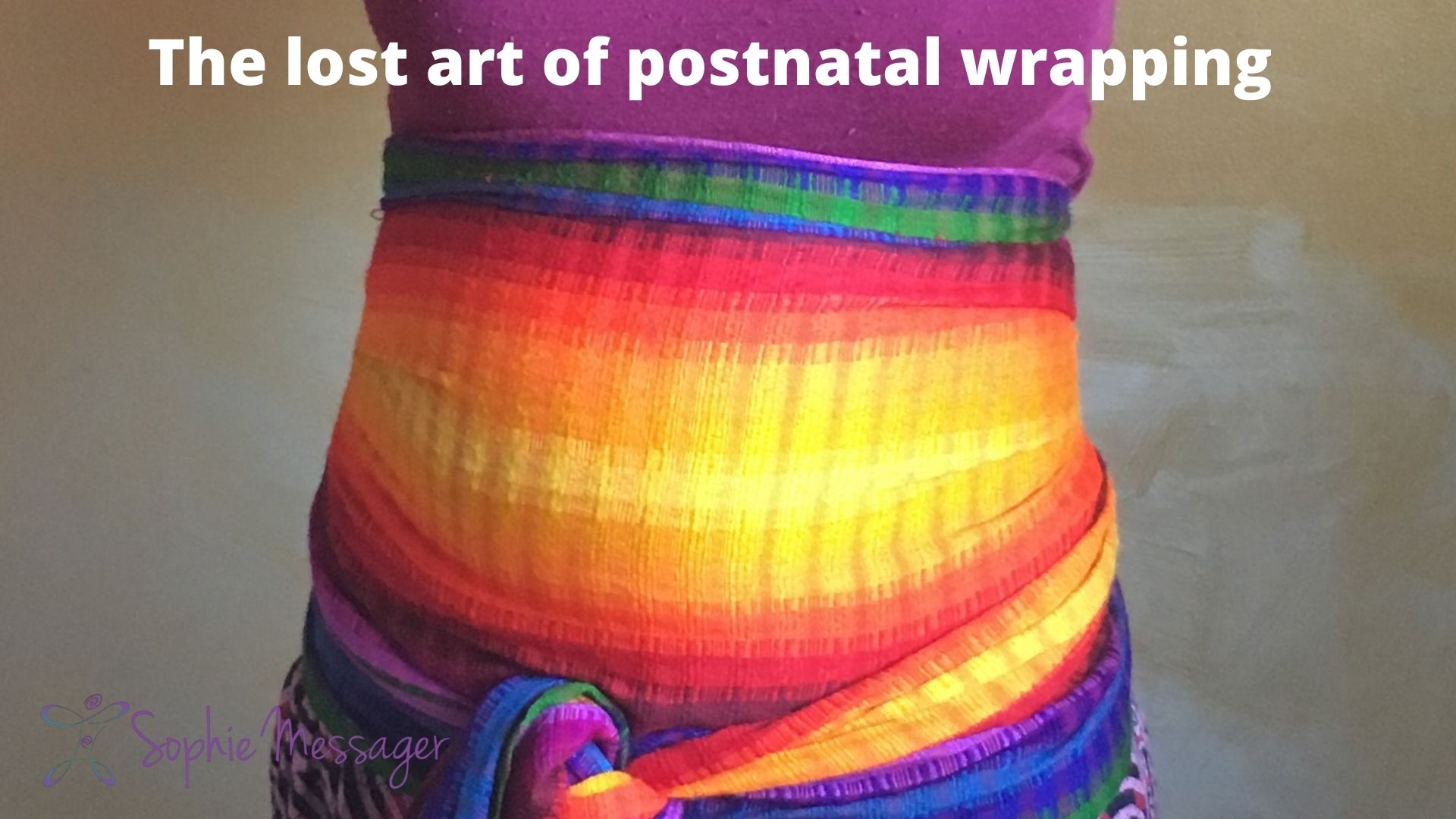
 New mothers are also open physically, emotionally and spiritually, and therefore the wrapping is part of the nurturing support to bring them back to their centre. On a simple physical level wrapping provides support to unstable joints and muscles. It also provides comfort and warmth. On an emotional level it brings us back to our bodies and provides a sense of being contained. On a spiritual level it feels containing and helps us come back to ourselves.
New mothers are also open physically, emotionally and spiritually, and therefore the wrapping is part of the nurturing support to bring them back to their centre. On a simple physical level wrapping provides support to unstable joints and muscles. It also provides comfort and warmth. On an emotional level it brings us back to our bodies and provides a sense of being contained. On a spiritual level it feels containing and helps us come back to ourselves. I see postpartum wrapping as a source of comfort, support and warmth. Done in accordance with the mother’s comfort and preferences, it can feel very good indeed.
I see postpartum wrapping as a source of comfort, support and warmth. Done in accordance with the mother’s comfort and preferences, it can feel very good indeed. With a very long, narrow cloth (about 15cm wide and 7 m long), you can do the Bengkung style binding, which goes from the hips to the ribs. Here is a video
With a very long, narrow cloth (about 15cm wide and 7 m long), you can do the Bengkung style binding, which goes from the hips to the ribs. Here is a video  How to choose the right way to wrap/bind for you?
How to choose the right way to wrap/bind for you?






